In the realm of human physiology, there exists a fascinating relationship between cortisol and the accumulation of fat in the abdominal region. This intricate connection, which plays a significant role in the development of abdominal obesity, has been a subject of keen interest among researchers and medical professionals alike.
It is vital to comprehend the intricate interplay between hormones and obesity, specifically in the context of cortisol and its effects on the waistline. Cortisol, often referred to as the stress hormone, is a powerful player in the intricate web of hormones that regulate various physiological processes within the human body. While cortisol serves essential functions such as regulating blood pressure and assisting in the immune response, its excessive secretion can wreak havoc on our waistlines.
A noteworthy aspect of cortisol’s impact on abdominal fat lies in its distinct influence on fat distribution across the body. While we might envision fat as a uniform entity, cortisol shapes its deposition with remarkable precision. Rather than accumulating evenly throughout the body, cortisol directs fat predominantly towards the abdominal region, leading to the infamous belly fat phenomenon.
Further comprehending the mechanisms by which cortisol influences abdominal obesity is of paramount importance, as it provides opportunities for interventions and the development of targeted strategies to combat this prevalent health issue. Gaining insight into how cortisol impacts our waistlines enables us to develop effective preventive and therapeutic interventions that can help individuals achieve and maintain a healthy body composition.
- The Impact of Cortisol on Belly Fat
- Exploring the Role of Hormones in Abdominal Obesity
- Understanding Cortisol: The Stress Hormone
- The Basics of Cortisol
- The Link between Cortisol and Abdominal Fat
- Effects of Chronic Stress on Cortisol Levels
- The Role of Hormones in Abdominal Obesity
- Hormonal Imbalances and Belly Fat Accumulation
- Impact of Insulin Resistance on Abdominal Fat Accumulation
- Questions and answers
The Impact of Cortisol on Belly Fat

Cortisol, a hormone produced by the adrenal glands, plays a crucial role in the accumulation of abdominal fat. This section explores the direct influence of cortisol on the development and persistence of belly fat, shedding light on the intricate relationship between this hormone and its impact on body composition.
| Effects of Elevated Cortisol Levels on Belly Fat | Mechanisms Behind Cortisol-induced Abdominal Obesity |
|---|---|
|
Increased cortisol levels have been strongly associated with greater accumulation of fat in the abdominal region. This phenomenon is often observed in individuals experiencing chronic stress, who tend to display a more prominent waist circumference and higher abdominal fat percentage. Elevated cortisol levels have been shown to lead to an increased desire for calorie-dense foods, especially those high in sugar and unhealthy fats. This combination can further contribute to the deposition of belly fat. Cortisol affects the distribution of fat in the body by promoting the storage of excess energy as visceral fat, which is particularly harmful to health. Visceral fat wraps around vital organs and has been linked to an increased risk of cardiovascular diseases, type 2 diabetes, and metabolic syndrome. |
The mechanisms behind cortisol-induced abdominal obesity are multifaceted. Cortisol activates lipoprotein lipase (LPL), an enzyme responsible for the uptake and storage of triglycerides in fat cells. The activation of LPL in adipose tissue enhances the deposition of fat, specifically in the abdominal area. Cortisol also impairs insulin sensitivity, leading to higher insulin production by the pancreas. Increased insulin levels promote the conversion of glucose into fat, favoring fat storage in the abdominal region. Furthermore, cortisol stimulates the breakdown of muscle tissue to provide amino acids for gluconeogenesis, a process that generates glucose. This muscle breakdown leads to a reduction in overall muscle mass, which in turn decreases energy expenditure and further contributes to abdominal fat accumulation. |
Understanding the detrimental impact of cortisol on belly fat can provide valuable insights into developing strategies for preventing and reducing abdominal obesity. Managing stress levels, adopting a healthy diet, incorporating regular exercise, and optimizing sleep patterns are all potential interventions that can help regulate cortisol levels and promote a healthier body composition.
Exploring the Role of Hormones in Abdominal Obesity

Investigating the Influence of Hormones on Excess Weight Around the Midsection
In this section, we delve into the intricate relationship between hormonal activity and the development of abdominal obesity. By examining the impact of hormones on the accumulation of fat in the abdominal region, we aim to shed light on the underlying mechanisms that contribute to this prevalent health concern. Through an exploration of various hormonal factors, we endeavor to provide a comprehensive understanding of how these substances influence the deposition and distribution of excess weight in the belly area.
An Intricate Balance
Understanding the role of hormones in abdominal obesity requires recognizing the delicate equilibrium that exists within the body’s endocrine system. Hormones such as cortisol, insulin, and leptin play a pivotal role in regulating various physiological processes, including metabolism, fat storage, and appetite control. Deviations in the levels or functioning of these hormones can disrupt the balance and lead to an increased tendency to accumulate fat in the abdominal region.
The Cortisol Connection
Cortisol, often referred to as the stress hormone, has garnered significant attention in discussions surrounding abdominal obesity. While cortisol serves important functions in the body’s stress response system, chronic or excessive secretion of this hormone can contribute to the accumulation of belly fat. By examining the influence of cortisol on adipose tissue distribution, we aim to unravel the complex relationship between chronic stress, hormonal activity, and abdominal obesity.
Insulin Resistance and Abdominal Fat
Another key hormone linked to abdominal obesity is insulin. Insulin resistance, a condition in which the body’s cells become less responsive to the effects of insulin, is closely associated with the deposition of fat in the abdominal area. By delving into the mechanisms behind insulin resistance and its impact on fat storage in the waistline, we aim to further comprehend the connection between hormone dysfunction and abdominal obesity.
Leptin and its Role in Abdominal Obesity
Leptin, a hormone secreted by fat cells, plays a crucial role in regulating appetite and energy balance. However, obese individuals often develop resistance to the effects of leptin, leading to disrupted appetite regulation and increased fat accumulation, particularly in the abdominal region. By examining the intricacies of leptin resistance and its association with abdominal obesity, we hope to enhance our understanding of the complex interplay between hormones and excess weight in the belly area.
Through this exploration of hormonal influences on abdominal obesity, we aim to broaden our comprehension of the underlying mechanisms and contribute to the development of effective strategies for prevention and treatment. By recognizing the role hormones play in shaping body composition, we can potentially pave the way for targeted interventions that address the specific hormonal disturbances associated with abdominal obesity.
Understanding Cortisol: The Stress Hormone
Cortisol, commonly known as the stress hormone, plays a significant role in our body’s response to stress and has a connection to abdominal obesity. By exploring the function and effects of cortisol, we can gain a better understanding of how this hormone influences our overall health and the accumulation of belly fat.
One of the key points to comprehend about cortisol is its association with stress. Although stress is a natural response to certain situations, chronic or prolonged stress can lead to an overproduction of cortisol. This excess cortisol can contribute to the storage of fat in the abdominal area, resulting in the development of belly fat.
Furthermore, cortisol also has an impact on various bodily functions beyond fat storage. It can influence appetite and cravings, leading to increased intake of high-calorie foods, often associated with abdominal obesity. Additionally, cortisol can affect metabolism, muscle breakdown, and insulin sensitivity, all of which can contribute to the accumulation of belly fat.
In order to understand the role of cortisol in abdominal obesity, it is necessary to consider the intricate relationship between hormones and the body’s physiological responses. By examining cortisol levels in individuals with abdominal obesity, researchers can gain insights into the complex mechanisms underlying this condition.
Overall, comprehending the role of cortisol, commonly referred to as the stress hormone, is crucial when exploring the connection between hormones and abdominal obesity. By examining its function, effects, and influence on various physiological processes, we can gain a deeper understanding of how cortisol contributes to the accumulation of belly fat and develop interventions to address this issue.
The Basics of Cortisol
In this section, we will delve into the fundamental aspects of cortisol, a hormone closely associated with abdominal obesity. By exploring the function and effects of cortisol, we can gain a deeper understanding of its role in the accumulation of belly fat.
Cortisol, commonly referred to as the stress hormone, plays a crucial role in various physiological processes within the body. It is produced by the adrenal glands and released in response to stress and low blood sugar levels. This hormone influences metabolism, immune response, and helps regulate blood pressure.
One of the primary functions of cortisol is to provide the body with a quick burst of energy in times of stress or danger. It achieves this by increasing glucose production and inhibiting insulin activity. Additionally, cortisol aids in the breakdown of proteins and fats, converting them into energy sources.
Chronically elevated levels of cortisol, however, can have negative effects on overall health and contribute to abdominal obesity. Prolonged exposure to stress and continuous production of cortisol can disrupt the balance of other hormones, such as insulin and leptin, which are involved in appetite regulation and fat storage.
Moreover, cortisol promotes the redistribution of fat to the abdominal region. Fat cells in this area have more receptors for cortisol than those in other parts of the body, making them susceptible to its effects. Increased cortisol levels can lead to the accumulation of visceral fat, which surrounds vital organs and poses greater health risks compared to subcutaneous fat.
Understanding the basics of cortisol is fundamental in exploring its role in abdominal obesity. By recognizing its functions and impact on fat storage, we can develop strategies to manage and mitigate the negative effects of chronically elevated levels of this hormone.
The Link between Cortisol and Abdominal Fat

Exploring the association between cortisol and abdominal fat sheds light on the impact of hormones in the accumulation of excess weight around the midsection. Cortisol, also known as the stress hormone, plays a significant role in regulating the body’s response to stress and maintaining homeostasis. This section delves into the intricate relationship between cortisol levels and abdominal obesity, highlighting the potential implications for individuals striving to reduce belly fat and improve overall health.
Effects of Chronic Stress on Cortisol Levels
Chronic stress has a profound impact on the levels of cortisol in the body, influencing its overall balance and functionality. This section explores the detrimental effects of prolonged stress on cortisol levels and how it can disrupt the delicate equilibrium of this essential hormone.
While cortisol serves as a crucial hormone in regulating various bodily processes, its excessive or prolonged release under chronic stress can lead to detrimental consequences. Elevated cortisol levels can negatively affect metabolism, immune function, cognition, and mood, among others.
Chronic stress triggers the hypothalamic-pituitary-adrenal (HPA) axis, activating a cascade of hormonal responses. This results in the release of cortisol from the adrenal glands, fueling the body’s fight-or-flight response. However, when stress becomes chronic, the HPA axis becomes dysregulated, leading to sustained cortisol elevation.
One of the main implications of heightened cortisol levels due to chronic stress is the accumulation of abdominal fat, commonly referred to as belly fat. Cortisol promotes the mobilization of glucose and enhances fat storage in visceral adipose tissue, leading to an increase in central obesity. Additionally, cortisol can also interfere with appetite regulation, leading to overeating and further contributing to weight gain.
Not only does chronic stress disrupt cortisol balance and contribute to abdominal obesity, but it can also lead to a variety of other health issues. Persistently elevated cortisol levels have been linked to cardiovascular problems, impaired cognitive function, compromised immune response, and mood disorders such as anxiety and depression.
In conclusion, chronic stress exerts a significant influence on cortisol levels, disrupting its delicate equilibrium and leading to a range of adverse effects. Understanding the relationship between chronic stress and cortisol regulation is crucial for tackling abdominal obesity and mitigating the detrimental impact on overall health and well-being.
The Role of Hormones in Abdominal Obesity
Hormonal imbalances play a crucial role in the development and progression of abdominal obesity. The intricate interplay between various hormones within the body can significantly influence the accumulation of fat in the abdominal region.
One important hormone involved in abdominal obesity is cortisol, commonly known as the stress hormone. Elevated cortisol levels due to chronic stress can contribute to increased abdominal fat storage. Additionally, the body’s natural response to stress may lead to altered appetite patterns and a preference for calorie-dense foods, further exacerbating abdominal obesity.
Insulin, a hormone released by the pancreas to regulate blood sugar levels, is also intricately linked to abdominal obesity. Insulin resistance, a condition where cells no longer respond effectively to insulin, can lead to excess fat storage, especially in the abdominal area. This hormonal imbalance can result from factors such as a sedentary lifestyle, poor diet, and genetic predisposition.
Adiponectin, another hormone secreted by fat cells, plays a protective role in abdominal obesity. It aids in regulating blood sugar levels, promoting fat breakdown, and reducing inflammation. Low levels of adiponectin are associated with increased abdominal fat accumulation and a higher risk of developing obesity-related diseases.
Leptin, often referred to as the satiety hormone, helps regulate appetite and energy balance. Individuals with abdominal obesity often exhibit leptin resistance, resulting in decreased satiety signals and an increased desire for food. This imbalance further perpetuates the vicious cycle of weight gain and abdominal fat accumulation.
Furthermore, sex hormones, such as estrogen and testosterone, have been linked to abdominal obesity. Hormonal fluctuations during menopause or conditions like polycystic ovary syndrome (PCOS) can contribute to increased abdominal fat deposition in women. In men, lower testosterone levels have been associated with increased abdominal fat and a higher risk of developing metabolic disorders.
- In conclusion, the role of hormones in abdominal obesity is multifaceted and complex. Hormonal imbalances, stress, insulin resistance, and altered appetite regulation all contribute to the accumulation of fat in the abdominal region. Understanding these hormonal mechanisms is crucial in developing effective strategies for managing and preventing abdominal obesity.
Hormonal Imbalances and Belly Fat Accumulation
Hormonal imbalances play a significant role in the accumulation of belly fat. When the delicate equilibrium of hormones in the body is disrupted, it can lead to an increase in abdominal obesity. Various factors, such as stress, unhealthy lifestyle choices, and genetic predisposition, can contribute to these imbalances.
The body’s hormonal system is intricate, with each hormone having a specific function. When there is an imbalance in hormones like cortisol, insulin, estrogen, and testosterone, it can result in a higher tendency for fat storage in the abdominal region. For instance, elevated levels of cortisol, commonly known as the stress hormone, can promote the accumulation of visceral fat around the abdomen.
Furthermore, lifestyle factors such as a sedentary lifestyle and a diet rich in processed foods and sugary beverages can disrupt hormone levels, leading to belly fat accumulation. Lack of physical activity and excessive consumption of these unhealthy foods can contribute to imbalances in insulin, which can hinder the body’s ability to regulate blood sugar and store fat, particularly in the abdominal area.
In addition to that, certain hormonal conditions, such as polycystic ovary syndrome (PCOS) in women, can also contribute to the development of abdominal obesity. PCOS is characterized by hormonal imbalances, including elevated levels of insulin and androgens, which can lead to increased fat deposition in the abdominal region.
Addressing hormonal imbalances is crucial in reducing belly fat accumulation. This can be achieved through lifestyle modifications, including regular exercise, a balanced diet consisting of whole foods, and stress management techniques. Additionally, consulting with a healthcare professional to assess hormone levels and potential underlying conditions is recommended for a holistic approach to combat abdominal obesity.
Impact of Insulin Resistance on Abdominal Fat Accumulation
Insulin resistance plays a pivotal role in the development and progression of abdominal obesity. This condition, characterized by reduced sensitivity to insulin, can disrupt the delicate balance of hormonal regulation in the body, leading to the accumulation of excess fat in the abdominal region.
Insulin, a hormone secreted by the pancreas, is responsible for regulating blood glucose levels and facilitating the uptake of glucose into cells for energy production. However, when cells become resistant to the effects of insulin, glucose is unable to enter the cells effectively, resulting in high blood sugar levels.
As a compensatory mechanism, the pancreas produces more insulin to overcome this resistance. Elevated insulin levels in the bloodstream can stimulate the storage of fat, particularly in the abdominal area. This is because insulin promotes the synthesis and storage of triglycerides in adipose tissue, leading to an increase in abdominal fat deposits.
Furthermore, insulin resistance also affects the breakdown of stored fat. It hinders the action of lipolytic enzymes, which are responsible for breaking down triglycerides into free fatty acids that can be used as fuel. As a result, the body relies more on glucose for energy, further contributing to the formation of abdominal fat.
In addition to its direct impact on fat accumulation, insulin resistance also influences other hormone systems involved in abdominal obesity. It disrupts the normal secretion and signaling of adipokines, such as adiponectin and leptin, which are crucial for regulating appetite and metabolism. Dysregulation of these adipokines can lead to increased hunger, decreased energy expenditure, and altered fat distribution, all of which contribute to the development of abdominal obesity.
Overall, insulin resistance plays a significant role in the pathogenesis of abdominal obesity. Understanding the complex interplay between insulin, hormones, and fat accumulation in the abdominal region is crucial for developing effective strategies to manage and prevent this widespread health concern.
Questions and answers
What is cortisol?
Cortisol is a hormone produced by the adrenal glands that helps the body deal with stress. It is often referred to as the stress hormone.
Is there a connection between cortisol and belly fat?
Yes, there is a connection between cortisol and belly fat. High levels of cortisol can lead to an increase in abdominal fat accumulation.
How does cortisol contribute to abdominal obesity?
Cortisol contributes to abdominal obesity by increasing appetite, promoting the storage of fat in the abdominal area, and inhibiting the breakdown of fat in other parts of the body.
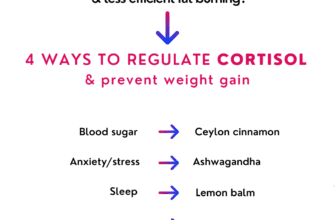
What are some ways to reduce cortisol levels?
There are several ways to reduce cortisol levels, including practicing stress management techniques such as meditation and yoga, getting regular exercise, getting enough sleep, and maintaining a healthy diet.
Can hormonal imbalance be a cause of abdominal obesity?
Yes, hormonal imbalance can be a cause of abdominal obesity. Imbalances in hormones such as cortisol, insulin, and estrogen can contribute to the accumulation of fat in the abdominal area.
What is the relationship between cortisol and belly fat?
Cortisol, also known as the stress hormone, plays a significant role in the accumulation of belly fat. When cortisol levels are elevated, it can lead to increased hunger, cravings for unhealthy foods, and the deposition of fat in the abdominal area.
How does cortisol affect hormone levels in the body?
Elevated cortisol levels can disrupt the balance of other hormones in the body. It can lead to lower levels of testosterone, which can decrease muscle mass and metabolism, and increased levels of insulin, which promotes fat storage.
Can high cortisol levels lead to weight gain?
Yes, high cortisol levels can contribute to weight gain, particularly in the abdominal area. Cortisol promotes the breakdown of muscle tissue and the accumulation of fat, especially around the midsection.
What are some strategies to reduce cortisol levels and combat belly fat?
There are several strategies to reduce cortisol levels and combat belly fat. These include practicing stress-reducing activities, getting adequate sleep, engaging in regular exercise, maintaining a healthy diet, and incorporating relaxation techniques such as meditation or deep breathing exercises.
Are there any specific foods or nutrients that can help regulate cortisol levels?
While there is no magic food or nutrient to specifically regulate cortisol levels, a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help promote overall hormonal balance, which may indirectly influence cortisol levels.