In the realm of mental and emotional well-being, certain factors often intertwine to shape an individual’s state of mind. Among the myriad contributors lies a particular hormone that, when imbalanced, may play a significant role in the development of mental health issues. This substance, commonly referred to as cortisol, has gained attention for its capacity to influence emotions and cognitive abilities.
Given its remarkable impact on the human psyche, a thorough examination of cortisol’s role is imperative in unraveling the complex web of stress, anxiety, and depression. By understanding the intricate connection between this stress hormone and mental health, one can begin to fathom the underlying mechanisms that contribute to the prevalence of psychological disorders in our society. Furthermore, exploring the relationship between cortisol and mood disorders may pave the way for new therapeutic approaches and interventions.
Deepening our comprehension of the intricate interplay between cortisol, anxiety, and low mood has the potential to unlock new insights into effective prevention and treatment strategies for individuals struggling with mental health challenges. By delving into the biochemistry and psychology behind this relationship, we can hope for a future where the burden of stress-related disorders is alleviated, and individuals can lead fulfilling lives.
- The Role of Cortisol in Mental Well-being: Investigating the Link between Stress and Depression
- Understanding Cortisol: The Stress Hormone
- Cortisol: Definition and Function
- Impact of Cortisol on the Brain
- How Stress Affects Cortisol Levels
- The Link Between Cortisol and Depression
- Cortisol Imbalance and Mood Disorders
- Cortisol and the Onset of Depression
- Chronic Stress, Cortisol, and Treatment-resistant Depression
- Questions and answers
The Role of Cortisol in Mental Well-being: Investigating the Link between Stress and Depression

In this section, we delve into the significant influence that cortisol, a hormone produced by the adrenal glands, has on an individual’s mental well-being. By examining the intricate relationship between the experience of stress and the development of depression, we aim to shed light on the multifaceted role played by cortisol in influencing mental health.
Cortisol, often referred to as the body’s primary stress hormone, is intricately interconnected with an individual’s response to stressors, both physiological and psychological. Elevated levels of cortisol in times of stress help mobilize the body’s resources, promoting a quick response to perceived threats. However, chronic exposure to stress and consequent persistent elevation of cortisol levels can have adverse effects on mental health, leading to the development of conditions such as depression.
The impact of cortisol on mental well-being is not limited to its role in the fight-or-flight response. This hormone is involved in regulating various bodily processes, including metabolism, immune function, and memory formation. Dysregulation of cortisol levels, whether chronically elevated or suppressed, can disrupt these essential functions and contribute to the onset and progression of mental health disorders.
Furthermore, the relationship between cortisol and depression is complex and bidirectional. While chronic stress can lead to elevated cortisol levels and increase the risk of developing depression, individuals with existing depression may exhibit abnormal cortisol patterns, such as decreased diurnal variation. Understanding this interplay between cortisol and depression can provide valuable insights into potential diagnostic and therapeutic interventions for individuals battling mental health conditions.
In summary, this section focuses on the crucial role that cortisol plays in mental well-being and explores the intricate connection between stress and depression. By comprehending the mechanisms through which cortisol influences mental health, we can develop a deeper understanding of the factors contributing to the development and management of depressive disorders.
Understanding Cortisol: The Stress Hormone
Exploring the intricate connection between stress and depression necessitates a comprehensive understanding of cortisol, commonly referred to as the stress hormone. This section aims to delve into the role of cortisol in mental health, shedding light on its impact and implications.
Cortisol, a hormone produced by the adrenal glands, plays a significant role in regulating various physiological processes in the human body. It is closely associated with the body’s stress response, acting as a vital alarm system for potential threats. When an individual experiences stress, cortisol levels rise, helping to mobilize energy reserves, increase focus and alertness, and enhance memory formation. However, prolonged or chronic stress can lead to persistent elevated cortisol levels, which can have detrimental effects on mental health.
High levels of cortisol have been linked to an increased risk of developing mental health disorders such as depression. Chronic stress and subsequent elevated cortisol levels can disrupt the balance of neurotransmitters in the brain, affecting mood regulation and leading to depressive symptoms. Moreover, cortisol can impair the functioning of the hippocampus, a brain region crucial for memory consolidation and emotional processing, further contributing to the development and progression of depression.
Understanding the intricate mechanisms through which cortisol influences mental health is crucial for developing effective interventions and treatment strategies for individuals experiencing stress and depression. By targeting cortisol regulation, researchers and healthcare professionals strive to mitigate the negative impact of chronic stress on mental well-being and improve treatment outcomes.
It is worth noting that while cortisol plays a crucial role in the stress response and mental health, it is only one piece of the larger puzzle. Various factors, including genetics, environment, and individual coping mechanisms, interact with cortisol to shape an individual’s overall mental health. By further exploring the complex interplay between cortisol and other contributing factors, researchers aim to develop a more comprehensive understanding of stress and depression, leading to enhanced prevention and treatment approaches.
In conclusion, comprehending the significance of cortisol, the stress hormone, is essential in unraveling the connection between stress and depression. By investigating its impact on the body and mental health, researchers can gain valuable insights into the underlying mechanisms and develop innovative approaches to support individuals experiencing the detrimental effects of chronic stress and depression.
Cortisol: Definition and Function
In the realm of mental health, an important factor that plays a significant role in the development and progression of stress and depression is a hormone known as cortisol. This hormone, which is naturally produced by our bodies, has various functions that impact our overall well-being and psychological state.
One of the key functions of cortisol is its involvement in the body’s stress response system. When we encounter a stressful situation, cortisol is released to help us cope with the challenge. It acts as a signal to alert our body to prepare for action, triggering a cascade of physiological changes that increase our energy levels and sharpen our focus. These changes can be essential when dealing with immediate threats or dangers.
Furthermore, cortisol also plays a vital role in regulating our sleep-wake cycle. It follows a diurnal pattern, with levels typically being highest in the morning and gradually declining throughout the day. This natural rhythm helps us feel more awake and alert in the morning, and gradually wind down for restful sleep at night. However, when this pattern is disrupted, such as in individuals experiencing chronic stress or depression, it can lead to difficulties in falling asleep, staying asleep, or experiencing poor-quality sleep.
In addition to its effects on stress and sleep, cortisol also influences various cognitive processes. It has been found to play a role in memory formation and retrieval, attention, and decision-making. However, excessive or prolonged exposure to cortisol can impair these cognitive functions, leading to difficulties with concentration, memory deficits, and reduced ability to make sound judgments.
Understanding the definition and function of cortisol provides insights into the intricate relationship between stress, depression, and mental health. By recognizing the impact of cortisol on these aspects, researchers and healthcare professionals can develop effective strategies to mitigate its negative effects and promote well-being in individuals struggling with stress and depression.
Impact of Cortisol on the Brain
The influence of cortisol on the brain is a significant area of research that explores the effects of this stress hormone on cognitive functioning and emotional well-being. Examining the relationship between cortisol levels and brain health provides valuable insights into the mechanisms behind stress-related disorders such as depression. By delving into the intricate workings of cortisol within the brain, researchers aim to understand how this hormone influences various aspects of mental and emotional functioning.
Studies have indicated that elevated levels of cortisol can have detrimental effects on brain structures involved in memory and emotional regulation. The prolonged exposure to high cortisol levels has been associated with shrinkage of the hippocampus, a region critical for memory consolidation and retrieval. Additionally, excessive cortisol can disrupt the functioning of the prefrontal cortex, a part of the brain responsible for executive functions such as decision-making, impulse control, and emotional regulation. These disruptions in brain structures can contribute to difficulties in memory, attention, and emotional stability, which are often observed in individuals experiencing chronic stress and depression.
Furthermore, cortisol has been found to impact the communication between different brain regions. Chronic exposure to elevated cortisol levels can disrupt the delicate balance of neurotransmitters, affecting their release and reception. This altered neurotransmitter activity can lead to imbalances in mood, contributing to the development and persistence of depressive symptoms. It also highlights the intricate interplay between cortisol and other neurotransmitter systems, such as serotonin and dopamine, which are closely linked to mood regulation.
Understanding the impact of cortisol on the brain is crucial for developing effective interventions and treatments for stress-related mental health disorders. By elucidating the precise mechanisms through which cortisol affects brain structures and functioning, researchers can potentially identify novel therapeutic targets. This knowledge can pave the way for the development of targeted interventions that aim to restore normal cortisol levels or mitigate the negative consequences of excessive cortisol on the brain, thereby improving mental well-being and quality of life for individuals affected by stress and depression.
How Stress Affects Cortisol Levels
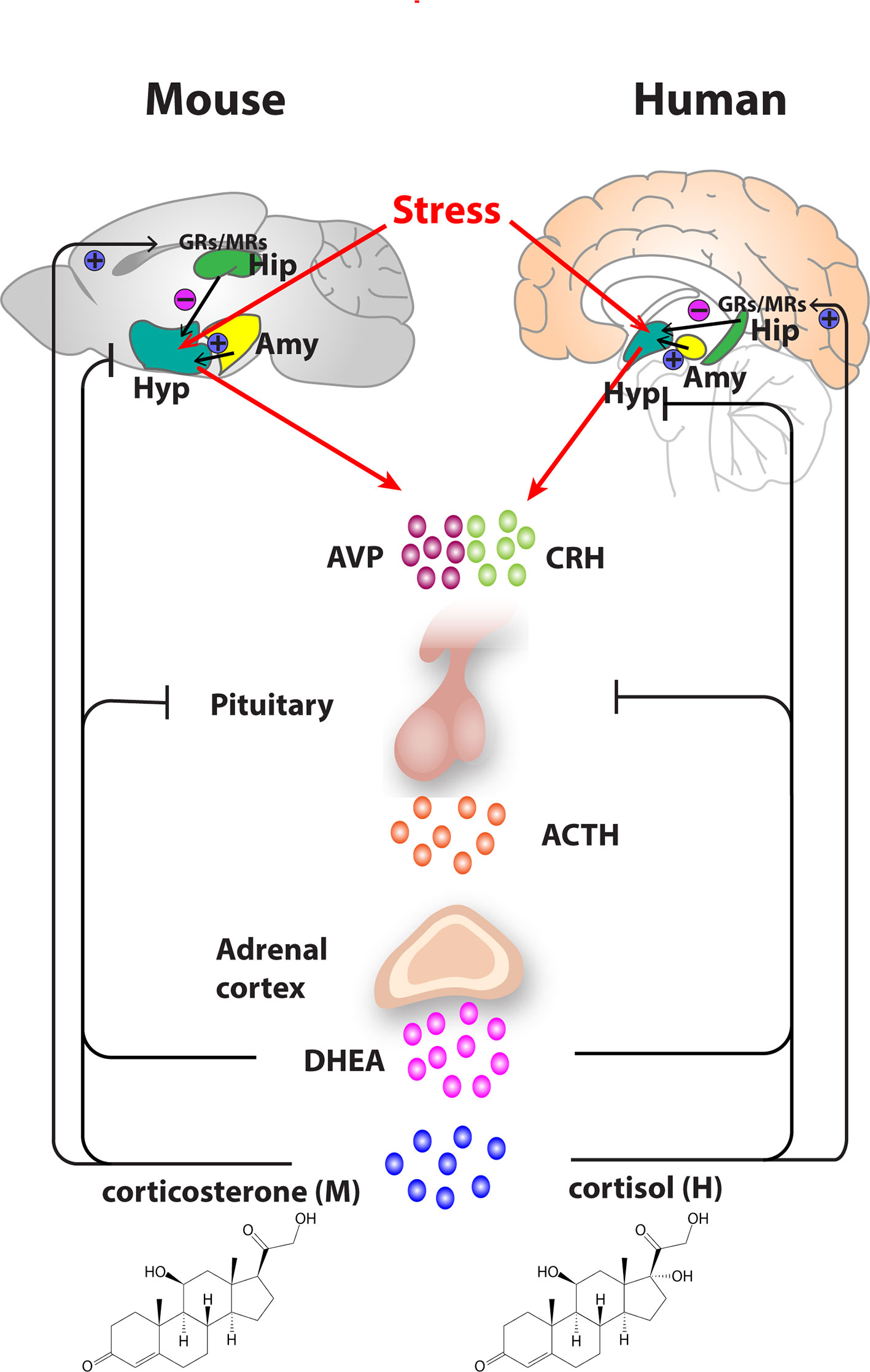
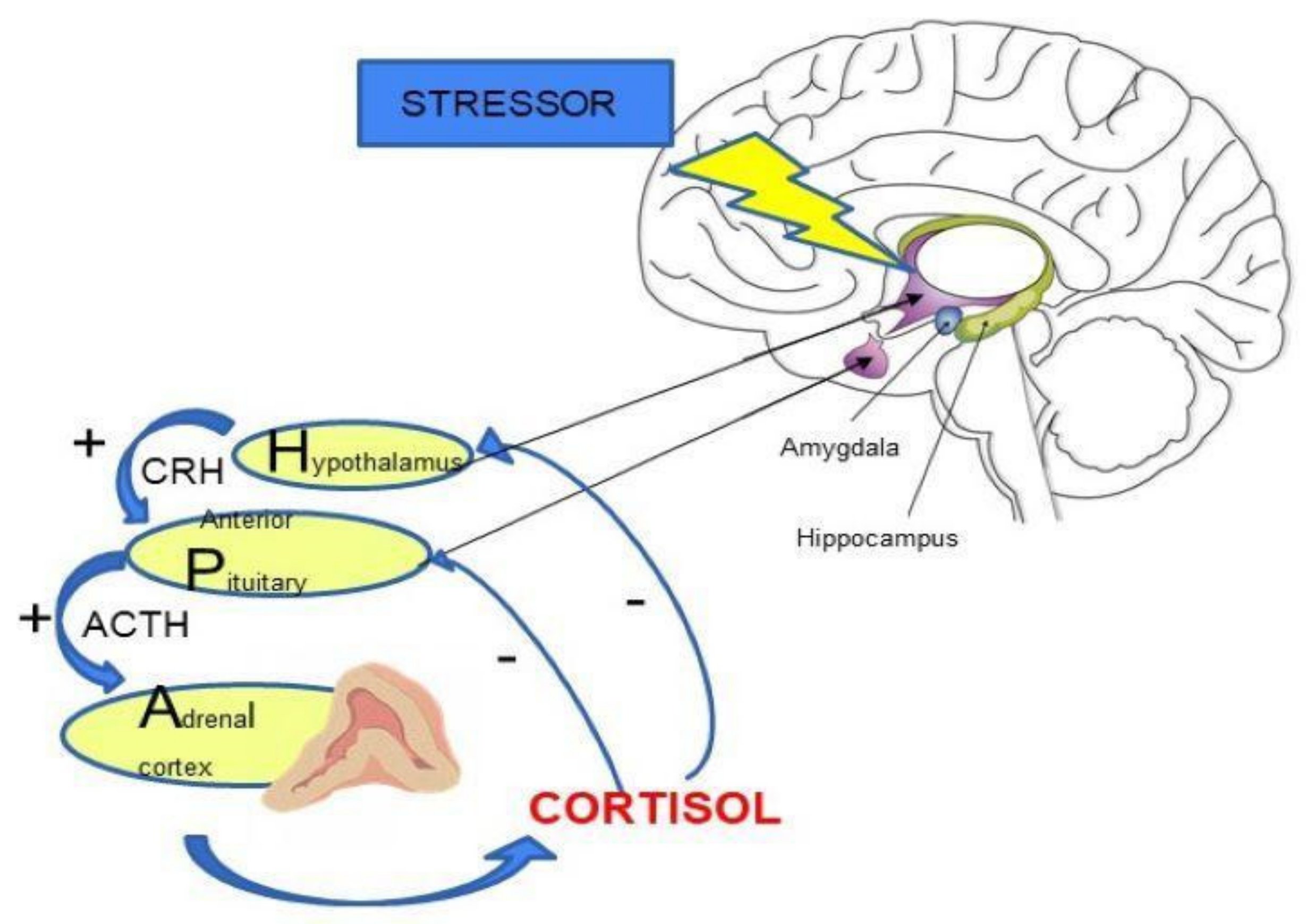
Experiencing periods of stress can have a significant impact on the levels of cortisol, a hormone produced by the adrenal glands in response to stress, in the body. The connection between stress and cortisol is complex and multifaceted, with stress triggering the release of cortisol into the bloodstream. This hormone plays a crucial role in various bodily functions, including metabolism, immune response, and the regulation of emotions.
When the body perceives stress, it initiates a cascade of physiological responses, resulting in the release of cortisol. This hormone helps the body cope with the stressor by mobilizing energy reserves and enhancing alertness. While cortisol is essential for survival in short-term stress situations, chronic stress can lead to elevated cortisol levels over an extended period.
Elevated cortisol levels resulting from chronic stress can have detrimental effects on mental health. Prolonged exposure to high levels of cortisol can disrupt the balance of neurotransmitters in the brain, contributing to the development of depression and other mood disorders. Additionally, cortisol can impair cognitive function, memory, and decision-making abilities.
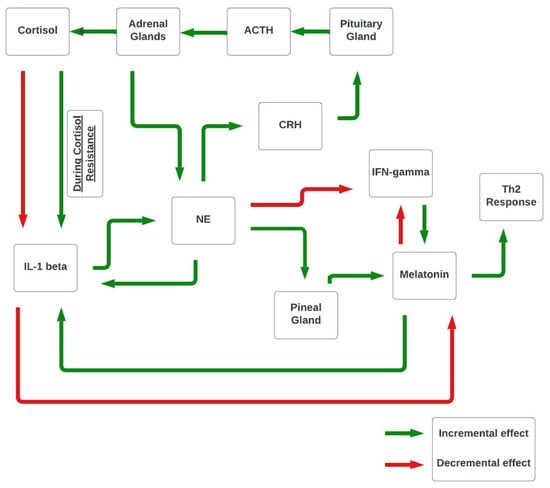
Furthermore, stress can also influence the regulation of cortisol levels through the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is a complex network involving the hypothalamus, pituitary gland, and adrenal glands, which controls the production and release of cortisol. Dysregulation of this system due to chronic stress can lead to disrupted cortisol patterns, with abnormal peaks and troughs throughout the day.
Understanding the intricate relationship between stress and cortisol levels is crucial in identifying potential interventions and treatments for mental health conditions such as depression. By recognizing the impact of stress on cortisol regulation, healthcare professionals can develop holistic approaches to managing stress and mitigating its detrimental effects on mental well-being.
The Link Between Cortisol and Depression
In this section, we will explore the intricate relationship between cortisol levels and depression, shedding light on the undeniable connection between these two significant factors. By delving into the physiological and psychological effects of cortisol, we aim to provide a comprehensive understanding of how this stress hormone contributes to the development and exacerbation of depression.
Research has consistently shown that elevated cortisol levels, typically associated with chronic stress, can have a detrimental impact on mental well-being. The excessive release of cortisol, often triggered by various stressors, disrupts the delicate balance of neurotransmitters in the brain, leading to depressive symptoms and mood disorders.
- 1. Cortisol’s influence on serotonin: Serotonin, known as the feel-good neurotransmitter, plays a crucial role in maintaining a stable mood. However, high cortisol levels can interfere with serotonin synthesis and its availability in the brain, leading to feelings of sadness and a higher susceptibility to depression.
- 2. The impact on hippocampal volume: The hippocampus is a vital brain structure involved in regulating emotions and memory formation. Chronic cortisol exposure can shrink the hippocampus, impairing its functions and contributing to the development of depressive symptoms.
- 3. Disrupted circadian rhythm: Cortisol follows a diurnal pattern, with levels peaking in the morning and gradually decreasing throughout the day. However, chronic stress can disrupt this natural rhythm, resulting in abnormal cortisol fluctuations. This disturbance can disrupt sleep patterns, worsen mood instability, and increase the risk of developing depression.
- 4. Cortisol and the immune system: Prolonged cortisol release can suppress the immune system, making individuals more vulnerable to infections and other illnesses. The resultant physical ailments can further exacerbate feelings of despair and hopelessness, contributing to the development of depression.
Understanding the link between cortisol and depression is of utmost importance in developing effective interventions and treatments. By recognizing the impact of cortisol on mental health, healthcare professionals can tailor therapeutic approaches that aim to regulate cortisol levels to alleviate depressive symptoms and promote overall well-being.
Cortisol Imbalance and Mood Disorders
A disrupted equilibrium of cortisol levels in the body can give rise to various types of mood disorders, impacting an individual’s emotional state and overall well-being. The intricate relationship between cortisol levels and mood disorders has been subject to extensive research and exploration. This section delves into the fundamental connection between imbalanced cortisol and the development of mood disorders.
Cortisol Dysregulation: The delicate balance of cortisol, a stress hormone produced by the adrenal glands, plays a critical role in maintaining emotional stability. An excess or deficiency of cortisol can lead to a wide array of mood disorders such as depression, anxiety, and bipolar disorder. This dysregulation disrupts the normal functioning of the brain and can result in significant changes to an individual’s mental state.
Mood Disorders and Cortisol: Elevated cortisol levels have been associated with an increased risk of developing mood disorders. Chronic stress, a significant contributor to cortisol imbalance, can trigger the onset of depression and anxiety. Similarly, low cortisol levels have also been linked to mood disorders, suggesting that both extremes can be detrimental to mental health.
The Neurobiological Impact: The impact of cortisol imbalance on mood disorders is intricately connected to the underlying neurobiology of the brain. Cortisol influences the activity of neurotransmitters, such as serotonin and dopamine, which play essential roles in regulating mood. Disruptions in cortisol levels can disturb the delicate interplay of these neurotransmitters, leading to imbalances that contribute to mood disorders.
Understanding the Role of Cortisol: Exploring the complex relationship between cortisol and mood disorders is crucial for gaining a comprehensive understanding of the underlying mechanisms of these conditions. By examining the role played by cortisol in the development and progression of mood disorders, researchers can pave the way for more informed interventions and treatments in the field of mental health.
Cortisol and the Onset of Depression
In this section, we delve into the correlation between cortisol, a stress hormone, and the development of depression. Our focus is on understanding how fluctuations in cortisol levels can contribute to the emergence of depressive symptoms.
Depression, a condition characterized by persistent feelings of sadness, loss of interest, and changes in behavior and cognitive function, is a widespread mental health issue affecting individuals around the globe. Research has shown that cortisol, a hormone naturally produced by the body in response to stress, plays a significant role in the development and progression of depression.
When faced with stressful situations, the body’s stress response system is activated, leading to an increase in cortisol release. This hormone, often referred to as the stress hormone, assists the body in managing stress by mobilizing energy resources and regulating various physiological functions. However, prolonged or chronic stress can disrupt the normal cortisol secretion pattern, resulting in excessive or insufficient levels of the hormone. These abnormal cortisol levels have been associated with an increased risk of developing depression.
Studies have indicated that individuals with depression tend to exhibit dysregulated cortisol levels, characterized by either sustained elevations or blunted secretion patterns throughout the day. High cortisol levels have been linked to an array of negative effects on mental health, including impairments in mood regulation and cognitive processes. On the other hand, low cortisol levels have been associated with decreased energy, concentration difficulties, and an overall sense of lethargy, all of which are commonly observed in individuals experiencing depression.
It is important to note that the relationship between cortisol and depression is complex and bi-directional. While chronic stress and elevated cortisol levels can contribute to the onset of depression, individuals with depression may also have pre-existing alterations in their cortisol function, predisposing them to higher susceptibility to stress. Understanding the intricate interplay between cortisol and depression is crucial for the development of effective interventions and treatments targeting this mental health condition.
Chronic Stress, Cortisol, and Treatment-resistant Depression
In this section, we delve into the persistent and prolonged pressure that individuals experience on a daily basis, referred to as chronic stress. We explore the intricate relationship between chronic stress, the hormone cortisol, and the complex nature of treatment-resistant depression. By analyzing the interplay between these factors, we aim to shed light on the challenges faced by individuals seeking effective treatment for their depression.
Chronic stress, characterized by ongoing and unrelenting psychological or environmental demands, places a significant burden on the body and mind. Its detrimental effects can manifest in various ways, including altered hormone levels and impaired mental well-being. One key hormone affected by chronic stress is cortisol, which plays a crucial role in regulating stress responses. Elevated levels of cortisol have been observed in individuals exposed to chronic stress, potentially contributing to the development or exacerbation of depression symptoms.
Treatment-resistant depression presents a formidable challenge for healthcare professionals and individuals alike. Despite numerous treatment options available, some individuals fail to respond adequately or at all to traditional interventions. This section explores the potential connection between chronic stress, elevated cortisol levels, and the development of treatment-resistant depression. By understanding this intricate relationship, researchers and clinicians can develop more effective strategies to address this complex and challenging mental health condition.
Questions and answers
How does cortisol impact mental health?
Cortisol, commonly known as the stress hormone, plays a significant role in mental health. When levels of cortisol are excessively high, it can lead to a series of negative effects on the brain, increasing the risk of mental health disorders such as depression.
Is there a connection between stress and depression?
Yes, there is a strong connection between stress and depression. Chronic or intense stress can disrupt the normal functioning of the brain, affecting neurotransmitters and hormones, including cortisol. This disruption can contribute to the development or worsening of depressive symptoms.
Can cortisol levels be linked to the development of mental health disorders?
Yes, elevated cortisol levels have been associated with an increased risk of developing mental health disorders, including depression. Prolonged exposure to stress and subsequent overproduction of cortisol can adversely affect the brain’s structure and function, influencing mood regulation and increasing vulnerability to psychiatric illnesses.
Are there any ways to reduce cortisol levels and alleviate mental health symptoms?
Yes, there are several strategies that can help reduce cortisol levels and alleviate mental health symptoms. These include practicing stress management techniques such as mindfulness meditation, engaging in regular exercise, getting adequate sleep, and seeking support from a mental health professional who can provide therapy or medication if necessary.
What are the long-term effects of chronically elevated cortisol levels on mental health?
Chronically elevated cortisol levels can have profound long-term effects on mental health. It can lead to the development of mood disorders, increased anxiety, impaired cognitive function, memory problems, decreased resilience to stress, and even structural changes in the brain. It is essential to address chronic stress and cortisol dysregulation to prevent or manage mental health conditions effectively.
What is cortisol and how does it affect mental health?
Cortisol is a hormone that is released by the body in response to stress. It can have both positive and negative effects on mental health. In short-term stress situations, cortisol helps the body to respond effectively and cope with the stress. However, chronic stress can lead to chronically elevated cortisol levels, which can contribute to the development of mental health issues such as depression.
Can high levels of cortisol lead to depression?
Yes, prolonged exposure to high levels of cortisol can increase the risk of developing depression. When cortisol levels remain consistently elevated due to chronic stress, it can disrupt the normal functioning of the brain and negatively impact mood regulation. Over time, this can contribute to the development of depressive symptoms.
What are the symptoms of excessive cortisol production?
Excessive cortisol production can manifest through various physical and psychological symptoms. Physical symptoms may include weight gain, especially in the abdominal area, high blood pressure, and increased susceptibility to infections. Psychological symptoms may include irritability, anxiety, difficulty concentrating, and changes in sleep patterns.
Can reducing stress levels help regulate cortisol and improve mental health?
Yes, reducing stress levels can help regulate cortisol production and have a positive impact on mental health. Engaging in stress-reducing activities such as exercise, meditation, or therapy can help lower cortisol levels. By reducing chronic stress, individuals may experience an improvement in their overall mood and decrease the risk of developing mental health issues related to elevated cortisol levels.
Are there any medical treatments available to regulate cortisol levels in individuals with mental health issues?
Yes, there are medical treatments available to regulate cortisol levels in individuals with mental health issues. In some cases, healthcare professionals may prescribe medication, such as cortisol-lowering drugs or antidepressants, to help regulate cortisol production and manage symptoms of depression or other mental health conditions. However, medication should always be used in conjunction with other forms of treatment, such as therapy or lifestyle changes, for optimal results.