Within the realm of physiological complexity, a perplexing enigma resides – immune system dysfunctions. Behind this intricate web of conditions lies a collection of disorders that challenge our understanding and compromise the delicate balance of our bodies. Despite the struggles faced by those afflicted with autoimmune diseases, there is hope in the ongoing quest to decipher their origins and develop effective management strategies.
Undoubtedly, one of the key hurdles in tackling autoimmune disorders lies in their identification. These enigmatic conditions manifest themselves through a myriad of symptoms, often nebulous and non-specific. By paying heed to subtle red flags and familiarizing oneself with the telltale signs, individuals can embark on a journey of recognition and better understand the complex interplay between their immune system and overall well-being.
Recognizing the Silent Whispers: Unmasking the Elusive Symptoms
Autoimmune diseases possess an uncanny ability to mimic various ailments, making them elusive and arduous to pinpoint. The body’s own immunity, once a safeguard, turns into a double-edged sword that attacks its own tissues and organs, eluding concrete diagnoses. Precarious sensations, lethargy, joint pain, skin rashes, and gastrointestinal disturbances emerge as mere whispers, painting an ambiguous canvas of symptoms that necessitate careful scrutiny.
Peering Through the Veil: Delving into Diagnostic Modalities
Demystifying autoimmune disorders hinges on unraveling their intricate layers through diagnostic tests and screening procedures. Propelling us closer to the truth, these modalities empower healthcare professionals with the tools to differentiate between underlying autoimmune processes and other health concerns. Armed with a comprehensive understanding of the diagnostic approaches available, individuals can embark on a journey of self-discovery and collaborate with their healthcare providers to find solace amidst the labyrinth of symptoms.
- Understanding Autoimmune Diseases: The Key to Diagnosis and Treatment
- Identifying Autoimmune Disease: Unmasking the Hidden Symptoms
- Unexplained Fatigue: A Red Flag for Autoimmune Disorders
- Skin Manifestations: Revealing the External Clues of Autoimmunity
- Joint Pain and Inflammation: A Common Denominator in Autoimmune Conditions
- Managing Autoimmune Disease: Navigating the Complexities of Treatment
- Lifestyle Modifications: Harnessing the Power of Nutrition and Exercise
- Medication and Therapy: Balancing the Immune System’s Response
- Seeking Support: The Significance of Emotional Well-being in Autoimmunity
- Questions and answers
Understanding Autoimmune Diseases: The Key to Diagnosis and Treatment
Comprehending Autoimmune Disorders: Unlocking the Essential Elements for Diagnosis and Management
Autoimmune diseases, an enigma of the human body, hold the secret to a multitude of symptoms and conditions that affect millions worldwide. A deeper understanding of these complex diseases is vital for accurate diagnosis and effective treatment. By unraveling the underlying mechanisms, healthcare professionals can identify the telltale signs and develop targeted approaches for managing autoimmune diseases.
An autoimmune disease occurs when the immune system, designed to protect the body, mistakenly attacks its own healthy cells and tissues. This disruption in the body’s self-recognition mechanism results in a cascade of immune responses that can lead to inflammation and damage throughout various organs or systems. The diverse nature of autoimmune diseases makes diagnosis challenging, as symptoms can vary widely and mimic other conditions. However, by recognizing the common patterns and characteristic signs, medical professionals can navigate the intricate web of symptoms and provide accurate diagnoses.
A comprehensive approach to the diagnosis and treatment of autoimmune diseases involves various diagnostic tools and techniques. From comprehensive medical history evaluations to extensive laboratory tests, healthcare providers carefully analyze the patient’s symptoms, medical records, and test results. This meticulous approach allows for the identification of specific antibodies and biomarkers that indicate the presence of autoimmune diseases, aiding in accurate diagnosis.
Once a diagnosis is made, the focus shifts towards developing a personalized treatment plan, aimed at managing the symptoms, slowing down disease progression, and minimizing tissue damage. Depending on the specific autoimmune disease, treatment options may include immunosuppressive medications, anti-inflammatory drugs, and lifestyle modifications. Close monitoring and regular follow-ups are essential to track the effectiveness of the chosen treatment plan and make necessary adjustments.
In conclusion, understanding autoimmune diseases is of utmost importance in successfully diagnosing and managing these complex conditions. By unraveling the underlying mechanisms and recognizing the common signs, healthcare professionals can pave the way to accurate diagnosis and effective treatment, ultimately improving the quality of life for individuals living with autoimmune diseases.
| Key Takeaways: |
|---|
| Autoimmune diseases involve the immune system mistakenly attacking healthy cells and tissues. |
| Accurate diagnosis requires recognizing common patterns and signs. |
| Diagnostic tools and techniques, such as medical history evaluations and laboratory tests, aid in identification. |
| Personalized treatment plans aim to manage symptoms and minimize tissue damage. |
| Regular monitoring and follow-ups are crucial for tracking treatment effectiveness. |
Identifying Autoimmune Disease: Unmasking the Hidden Symptoms
Exploring the Enigma of Autoimmune Conditions: Revealing the Elusive Indicators
In this section, we delve into the perplexing realm of autoimmune diseases. Unveiling the enigmatic nature of these conditions, we aim to shed light on the often hidden symptoms that can signal their presence. By understanding the subtle clues that the body provides, we can better identify and address autoimmune diseases at their early stages.
- Unmask the Cryptic: Unraveling the Veiled Manifestations
- Raising Awareness: Spotting the Unusual Red Flags
- Decoding the Silent Clues: Recognizing the Muted Signs
- Unveiling the Masquerade: Identifying the Camouflaged Indications
- Be Informed: Familiarizing Yourself with the Subtle Warnings
It is crucial to be cognizant of the concealed symptoms that autoimmune diseases can present. By developing a knowledge base around these less obvious signs, individuals and healthcare professionals can work together to bring about early detection and appropriate management strategies. Let us embark on this journey of unwrapping the hidden symptoms that can unmask the presence of autoimmune diseases.
Unexplained Fatigue: A Red Flag for Autoimmune Disorders

Unexplained exhaustion that persists despite adequate rest and sleep can be a significant indicator of underlying autoimmune disorders. Fatigue, beyond regular tiredness, can be a subtle yet crucial sign that something is amiss within the body’s immune system.
Unbeknownst to many, extreme weariness can be an early warning signal of an underlying autoimmune condition. This persistent feeling of tiredness is not relieved by rest or sleep and can have a debilitating impact on an individual’s daily life. While fatigue itself is a rather common complaint, the unexplained nature of this exhaustion becomes a red flag when considering the possibility of autoimmune disorders.
Autoimmune disorders occur when the body’s immune system mistakenly attacks its own healthy cells and tissues, leading to chronic inflammation and various adverse effects. Unexplained fatigue often emerges as one of the initial symptoms, serving as a subtle indication of an immune system in distress.
It is important not to dismiss unexplained fatigue as a temporary or insignificant concern. Recognizing it as a potential red flag for autoimmune disorders can prompt individuals to seek timely medical evaluation and intervention. By addressing the underlying autoimmune condition, not only can the fatigue be alleviated, but the overall quality of life can improve significantly.
If you find yourself experiencing unexplained fatigue that persists for an extended duration, it is crucial to consult with a healthcare professional. They can conduct the necessary assessments, such as blood tests and medical history evaluation, to determine if an autoimmune disorder may be the underlying cause. Early detection and treatment offer the best chances for effectively managing autoimmune disorders and mitigating their impact on daily life.
In conclusion, unexplained fatigue serves as a red flag for autoimmune disorders and should not be ignored. It is essential to recognize this symptom as a potential indication of underlying immune system dysfunction and seek medical evaluation promptly. By addressing the root cause, individuals can take necessary steps towards managing their condition and improving their overall well-being.
Skin Manifestations: Revealing the External Clues of Autoimmunity
The skin often holds the key to unraveling the intricate puzzle of autoimmune diseases. A close examination of the external manifestations on the skin can provide valuable clues about underlying autoimmunity, offering valuable insights into the diagnosis and management of these conditions.
Through careful observation of the skin’s appearance, texture, and abnormal features, medical professionals can gain significant insights into the potential presence of autoimmune diseases. Skin manifestations can vary widely, presenting as rashes, ulcers, discoloration, or even lesions that may appear and disappear over time. These external signs can serve as an early warning system, indicating the need for further investigation and prompt intervention.
Furthermore, understanding the different types of skin manifestations associated with specific autoimmune diseases is crucial for accurate diagnosis and effective management. Conditions such as psoriasis, lupus, and dermatomyositis often manifest unique patterns and characteristics on the skin, providing diagnostic clues for healthcare professionals trained to recognize these telltale signs.
While the external clues of autoimmunity are evident on the skin, it is vital to emphasize that these manifestations are not merely superficial. They reflect the complex interplay of the immune system, genetics, and environmental factors within the body. Proper recognition and interpretation of these external signs can guide medical professionals towards personalized treatment approaches that target the underlying autoimmune mechanisms.
By discussing the significance of skin manifestations in autoimmunity, this article aims to shed light on the importance of paying attention to external clues. It underscores the necessity of collaboration between patients, dermatologists, and rheumatologists to recognize, evaluate, and manage the skin manifestations associated with autoimmune diseases effectively.
Joint Pain and Inflammation: A Common Denominator in Autoimmune Conditions
Understanding the relationship between joint pain and inflammation is crucial in unraveling the complexities of autoimmune conditions. In these conditions, the body’s immune system mistakenly attacks its own healthy tissues, leading to chronic inflammation and joint pain. This article delves into the significance of joint pain and inflammation as a common factor in diverse autoimmune diseases, shedding light on their underlying mechanisms and providing insights into effective management strategies.
Understanding the intricacies involved in effectively managing autoimmune diseases is paramount for individuals seeking to regain control over their health. This article explores the complex nature of treatment options and provides practical insights to help patients navigate through this challenging journey.
1. Embracing personalized care: Each individual’s experience with autoimmune disease is unique, requiring a tailored approach to treatment. By working closely with healthcare professionals, patients can identify specific triggers, symptoms, and potential treatment options that align with their personal needs.
2. Building a comprehensive treatment plan: Managing autoimmune disease often involves a multifaceted strategy integrating medication, lifestyle modifications, stress reduction techniques, and complementary therapies. By compiling a comprehensive treatment plan that takes into account all aspects of a patient’s life, an effective management approach can be established.
3. Prioritizing self-care: Navigating the complexities of autoimmune disease requires individuals to prioritize self-care. This involves adopting healthy lifestyle habits, such as regular exercise, a balanced diet, quality sleep, and stress management techniques. Investing in self-care not only promotes overall well-being but also strengthens the body’s ability to manage the effects of the disease.
4. Educating oneself: Taking an active role in understanding the intricacies of autoimmune disease empowers individuals to make informed decisions about their health. By staying updated on the latest research, treatment options, and support resources, patients can better advocate for themselves and actively participate in their treatment journey.
5. Seeking support: Living with an autoimmune disease can be emotionally challenging. Connecting with support groups, online communities, and counseling services can provide individuals with the necessary emotional support and empathy. Sharing experiences and learning from others can help individuals navigate the complexities of treatment and find solace in a community of individuals facing similar challenges.
By embracing personalized care, building a comprehensive treatment plan, prioritizing self-care, educating oneself, and seeking support, individuals can effectively manage autoimmune diseases and lead fulfilling lives. While the journey may be complex, with the right tools and support, individuals can navigate through the challenges and regain control over their health.
Lifestyle Modifications: Harnessing the Power of Nutrition and Exercise

Embracing a holistic approach to health and well-being, this section explores the potential impact of lifestyle modifications, specifically focusing on the power of nutrition and exercise. By acknowledging the profound influence that our daily choices can have on our immune system, we can proactively take steps to optimize our overall health and potentially manage autoimmune conditions.
Nutrition:
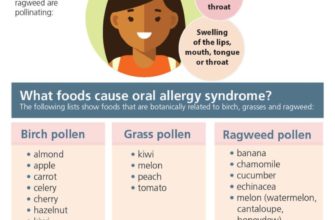
Food is not merely fuel for our bodies; it can also serve as a powerful tool in promoting and maintaining optimal health. By making intentional choices to nourish our bodies with nutrient-dense foods, we can support our immune system and potentially alleviate the burden of autoimmune diseases. A diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and healthy fats, can help modulate our immune response and reduce inflammation. Additionally, incorporating specific nutrients, such as omega-3 fatty acids, vitamin D, and antioxidants, may provide further support in managing autoimmune conditions.
Exercise:
Regular physical activity not only enhances our cardiovascular health and muscular strength but also plays a crucial role in supporting our immune system. Engaging in aerobic exercises, such as brisk walking, cycling, or swimming, can improve blood circulation, promote the production of endorphins, and reduce inflammatory markers. Furthermore, incorporating strength training exercises helps maintain muscle mass and bone density, both of which are essential in supporting overall health and immune function. It is important to find activities and exercise routines that are enjoyable and sustainable, as consistency is key to reaping the benefits.
Lifestyle Integration:
Adopting a conscious and sustainable approach to lifestyle modifications can greatly impact our overall well-being and potentially mitigate the symptoms of autoimmune diseases. Harnessing the power of nutrition and exercise requires a holistic mindset, recognizing that our choices extend beyond what is on our plate or the time we spend working out. Prioritizing stress management techniques, such as mindfulness practices, adequate sleep, and fostering a positive support system, are equally important. By implementing these changes gradually and customizing them to suit individual needs, we can synergistically cultivate a lifestyle that optimizes our immune system and promotes long-term health.
Medication and Therapy: Balancing the Immune System’s Response
In this section, we will explore the various approaches to managing autoimmune diseases by focusing on medication and therapy options that aim to achieve a delicate equilibrium in the immune system’s reaction.
When it comes to combating autoimmune disorders, finding the right balance is crucial. Medications play a vital role in this process by helping to regulate and modulate the immune system’s response. These medications, prescribed by healthcare professionals, target specific components of the immune system, aiming to either curb its hyperactivity or provide support when it is underactive.
Immunosuppressants, for example, are often prescribed to dampen an overactive immune system. By reducing the immune response, these medications help alleviate symptoms and prevent further damage to the body’s own tissues. On the other hand, immunostimulants can be used to boost a weakened immune system, effectively enhancing its ability to fight off infections and manage autoimmune processes.
Alongside medication, various therapies complement and enhance the immune system’s balance. Physical therapy aims to improve mobility and strength, helping individuals with autoimmune diseases to maintain an active lifestyle while managing their condition. Additionally, occupational therapy focuses on assisting individuals in adapting to their specific autoimmune symptoms and challenges, empowering them to engage in daily activities effectively.
The role of psychological therapy should not be underestimated either. Autoimmune diseases often bring emotional and mental burdens, and addressing these aspects is crucial for overall well-being. Through counseling or support groups, individuals can gain valuable insights, coping strategies, and emotional support, enabling them to better navigate the challenges that autoimmune diseases present.
It is essential to remember that medications and therapies vary depending on the specific autoimmune disease and individual characteristics. Healthcare professionals, such as rheumatologists and immunologists, work closely with patients to develop personalized treatment plans that take into account both the physical and emotional components of their conditions.
In conclusion, achieving a balance in the immune system’s response is the key objective when managing autoimmune diseases. Through a combination of medication and various therapies, individuals can actively participate in the management of their conditions and improve their overall quality of life.
Seeking Support: The Significance of Emotional Well-being in Autoimmunity

Within the realm of autoimmunity, it is essential to recognize the weight of emotional well-being and the impact it can have on individuals facing this complex condition. This section aims to highlight the importance of seeking emotional support for those dealing with autoimmune diseases, emphasizing the significance of managing stress, maintaining a positive mindset, and fostering healthy coping mechanisms.
1. Recognizing the Emotional Impact: Autoimmune diseases present unique challenges, both physically and emotionally. The psychological toll can include feelings of anxiety, depression, and frustration. Acknowledging these emotions and understanding their impact is crucial in addressing the holistic well-being of individuals with autoimmune conditions.
2. The Role of Stress Management: Chronic stress can exacerbate autoimmunity symptoms and trigger flare-ups. Therefore, adopting effective stress management techniques such as meditation, yoga, or engaging in hobbies can significantly contribute to emotional well-being and alleviate the burden on the immune system.
3. Building a Support System: Surrounding oneself with a network of understanding and empathetic individuals can provide immense emotional support. This can be achieved through joining support groups, attending therapy sessions, or connecting with others who share similar experiences through online forums or social media platforms.
4. Exploring Healthy Coping Mechanisms: Engaging in activities that promote relaxation and self-care is vital in managing emotional well-being. This can involve practicing mindfulness, participating in creative outlets, or engaging in physical exercise, tailored to the individual’s capabilities and preferences.
5. Addressing the Stigma: Autoimmune diseases are often misunderstood, leading to social stigma and feelings of isolation. By raising awareness and promoting understanding, individuals can break the barriers and find the necessary emotional support they deserve.
In summary, recognizing the emotional impact, managing stress, building a support system, exploring healthy coping mechanisms, and addressing the stigma associated with autoimmune diseases are all crucial steps in prioritizing emotional well-being for individuals facing autoimmunity. Seeking support and focusing on this aspect of care can enhance overall quality of life and empower individuals on their journey toward managing and living well with autoimmune conditions.
Questions and answers
What are the telltale signs of autoimmune disease?
The telltale signs of autoimmune disease can vary depending on the specific condition, but common symptoms include fatigue, joint pain, muscle weakness, rashes, and fever.
How can autoimmune diseases be diagnosed?
Autoimmune diseases can be diagnosed through a combination of medical history, physical examination, blood tests to detect antibodies, and sometimes imaging tests like X-rays or MRIs.
What are the treatment options for autoimmune diseases?
Treatment for autoimmune diseases often involves a combination of medications to suppress the immune system and manage symptoms, lifestyle changes such as a healthy diet and exercise, and sometimes specialized therapies like physical therapy or counseling.
Are autoimmune diseases hereditary?
While the exact causes of autoimmune diseases are still not fully understood, there is evidence to suggest that genetics play a role. Having a family history of autoimmune diseases can increase the risk of developing one.
Can autoimmune diseases be cured?
Most autoimmune diseases cannot be cured, but they can be managed effectively with proper treatment and lifestyle modifications. The goal of treatment is usually to control symptoms, prevent flare-ups, and minimize long-term damage.
What are the common signs of autoimmune disease?
Common signs of autoimmune disease can include fatigue, joint pain, swelling, skin rashes, and digestive problems.
How can autoimmune diseases be diagnosed?
Autoimmune diseases can be diagnosed through a combination of medical history, physical examination, blood tests, and sometimes additional specialized tests like imaging or biopsies.
What are the treatment options for autoimmune diseases?
Treatment options for autoimmune diseases vary depending on the specific condition, but they may include medications to manage symptoms, immune-suppressing drugs, lifestyle changes, and in some cases, surgery.
Can autoimmune diseases be prevented?
While the exact causes of autoimmune diseases are not always known, there are some lifestyle factors that may help reduce the risk, such as maintaining a healthy diet, exercising regularly, managing stress, and avoiding exposure to environmental toxins.
Can autoimmune diseases affect any age group?
Autoimmune diseases can affect individuals of any age group, although certain conditions may be more common in certain age ranges. Some autoimmune diseases, such as rheumatoid arthritis, can develop in adulthood, while others, like type 1 diabetes, may appear in childhood.