Uncovering the concealed torment that lurks beneath the surface, we delve into the inconspicuous world of ailments that afflict the immune system. In this segment, we embark on an exploration of the subtle cues that manifest in individuals grappling with these enigmatic diseases. By raising awareness and understanding the telltale signals, we can alleviate the burden that comes with the excruciating battles fought within.
Within this realm of bodily intricacies, a clandestine adversary silently attacks the very essence of our humanity. Empower yourself with knowledge and become attuned to the cryptic whispers of your body, for it holds the key to unveiling the enigma that is autoimmune disease. Although elusive, its presence can be discerned through a series of subtle disturbances that evade the untrained eye.
Enter a world where whispers carry the weight of a scream, where imperceptible tremors mark the battlefield, and where the once harmonious symphony of the immune system falls into discord. Here, internal warriors embark on an unrelenting quest to protect, but in their zealousness, they inadvertently turn against the self they were designed to preserve. It is in this paradoxical dance that shadows of autoimmune disease emerge.
Distinguishable only by those who listen intently, the indications of autoimmune disease tiptoe through life, their arrival often dismissed as mere randomness. Yet, embedded within these fluctuations lie hints of a greater narrative that unfold in whispers and echoes. By unearthing the sly manifestations, we can diminish the silent suffering experienced by those whose bodies wage war against themselves, one cell at a time.
- Unveiling the Silent Suffering: Recognizing the Telltale Signs of Autoimmune Disease
- A Closer Look at Autoimmune Diseases
- Understanding the Body’s Betrayal
- The Prevalence of Autoimmune Diseases
- Identifying Common Symptoms
- Unexplained Fatigue: A Subtle Warning Sign
- Persistent Joint Pain: Uncovering the Root Cause
- Skin Problems: When Autoimmunity Takes Its Toll
- Diagnosing Autoimmune Diseases
- Questions and answers
Unveiling the Silent Suffering: Recognizing the Telltale Signs of Autoimmune Disease

Understanding the subtle hints and indications of autoimmune diseases is crucial for early detection and effective management. By deciphering the unspoken language of our bodies, we can unveil the hidden suffering caused by these complex disorders.
1. Unexplained Fatigue: Often mistaken for general tiredness, unexplained fatigue can be a red flag for autoimmune diseases. Individuals may experience a persistent lack of energy, even after ample rest, hindering their ability to carry out daily activities.
2. Joint and Muscle Pain: Unlike regular muscle soreness after exercise, persistent joint and muscle pain can signal the presence of an autoimmune disease. These types of discomfort often worsen with movement and may cause significant discomfort or restricted mobility.
3. Skin Issues: Various skin conditions can be indicative of an underlying autoimmune disorder. Rashes, hives, dryness, or discoloration that do not respond to typical treatments may require further investigation to determine if they are related to an autoimmune condition.
4. Digestive Disturbances: Frequent digestive issues, such as abdominal pain, bloating, diarrhea, or constipation, may be linked to autoimmune diseases like Crohn’s disease or celiac disease. Understanding these signs can lead to appropriate diagnostic tests and treatment plans.
5. Cognitive Difficulties: Memory problems, difficulty concentrating, and impaired cognitive function can occur with autoimmune diseases affecting the brain, such as multiple sclerosis or lupus. Recognizing these cognitive changes is crucial for early intervention and support.
6. Sensitivity to Temperature: Unusual sensitivity to hot or cold temperatures, extreme sweating, or difficulty regulating body temperature can indicate an autoimmune disorder impacting the regulation of the body’s thermostat. These symptoms should not be overlooked and may require consultations with medical professionals.
7. Swelling and Inflammation: Chronic inflammation and swelling, often seen in autoimmune diseases like rheumatoid arthritis, can affect various parts of the body, including joints, organs, and tissues. Identifying these telltale signs of inflammation is vital for initiating appropriate treatment strategies.
Recognizing these telltale signs and understanding the silent suffering caused by autoimmune diseases is crucial for early detection and timely intervention. Consulting with healthcare professionals and undergoing appropriate diagnostic tests can help individuals receive the necessary support and management to improve their quality of life.
A Closer Look at Autoimmune Diseases
Examining the intricate nature of autoimmune diseases, we delve into the depths of these hidden afflictions that wreak havoc on the body’s own defense mechanisms. Shedding light on the enigmatic enigma that is autoimmune diseases, we aim to provide a comprehensive understanding of their underlying mechanisms, impact, and the importance of early recognition.
A Complex Web of Internal Struggles
Within the vast realm of the human body, an intricate battle ensues, as the immune system mistakenly recognizes the body’s own tissues as foreign invaders. This self-inflicted confusion unleashes a cascade of immune responses, ultimately leading to the development of autoimmune diseases.
From rheumatoid arthritis that attacks the joints to multiple sclerosis that affects the nervous system, autoimmune diseases manifest in a myriad of ways, each with their own set of telltale signs and symptoms.
An Unseen Enemy
Unfortunately, autoimmune diseases often operate in silence, masquerading as other ailments or remaining undetectable altogether. Their covert nature obscures the suffering experienced by those afflicted, leading to delayed diagnoses and prolonged discomfort.
It is crucial, therefore, to shed light on the intricacies of autoimmune diseases and equip individuals with the knowledge to recognize the subtle red flags that may indicate their presence.
Pioneering Early Detection and Treatment Strategies
Recognizing the importance of early detection, researchers and medical professionals are tirelessly working towards developing innovative techniques for diagnosing and managing autoimmune diseases. Through cutting-edge research and advancements in technology, we can empower patients with timely interventions and personalized treatment plans.
By unraveling the mysteries surrounding autoimmune diseases and promoting awareness, we pave the way for better understanding, improved outcomes, and enhanced quality of life for those grappling with these silent afflictions.
Understanding the Body’s Betrayal
A deeper understanding of the body’s betrayal requires an exploration of the intricate mechanisms that govern our immune system. Complex biological processes and interplay of cells, antibodies, and proteins contribute to the delicate balance of self-tolerance, which is disrupted in autoimmune diseases. Through a comprehensive examination, we can begin to comprehend the underlying causes and triggers that lead to this self-sabotaging phenomenon.
Furthermore, we shed light on the diverse array of autoimmune diseases that afflict individuals worldwide. Rheumatoid arthritis, multiple sclerosis, lupus, and type 1 diabetes are just a few examples of conditions in which the body’s immune system launches unwarranted attacks on healthy tissues. By exploring these diseases in detail, we can identify the unique signs and symptoms associated with each condition, enabling early intervention and optimal treatment.
The consequences of autoimmune diseases extend far beyond the physical realm. They can negatively impact one’s quality of life, causing chronic pain, fatigue, and emotional distress. By recognizing the silent suffering experienced by individuals with autoimmune diseases, we can promote empathy, support, and understanding within society, creating a nurturing environment for those affected.
| Key Points Covered: |
|---|
| – Body’s immune system turning against its own tissues and organs |
| – Complex mechanisms underlying autoimmune diseases |
| – Exploration of specific autoimmune conditions and their symptoms |
| – Impact of autoimmune diseases on quality of life |
The Prevalence of Autoimmune Diseases

Understanding the widespread occurrence of autoimmune diseases is crucial in addressing and managing these complex conditions. Autoimmune diseases, which encompass a diverse range of disorders, affect a considerable number of individuals worldwide. These conditions arise when the immune system, which normally protects the body from foreign invaders, mistakenly attacks its own healthy tissues and organs. To comprehend the impact and significance of autoimmune diseases, it is essential to explore their prevalence and the implications they carry.
Scope of the Problem
An alarming number of individuals worldwide, spanning various age groups and demographics, suffer from autoimmune diseases. These conditions are not limited to a specific region or population, affecting people globally. Due to their hidden nature, autoimmune diseases often go undiagnosed or misdiagnosed for years, leading to prolonged suffering and increased healthcare burden. The wide range of symptoms and variability in disease progression further complicates accurate diagnosis and assessment of their prevalence.
Statistics and Impact
While exact figures may vary, autoimmune diseases collectively impact millions of people globally. Numerous studies and research efforts have allowed us to gain insights into their prevalence. It is estimated that as many as 50 million people in the United States alone are affected by autoimmune diseases, making these conditions a significant public health concern.
Moreover, the impact of autoimmune diseases extends beyond the individuals directly affected by the conditions. Their effects ripple through families, friends, and communities, as caregivers and loved ones provide support and navigate the challenges posed by these chronic illnesses. Additionally, autoimmune diseases impose a considerable economic burden, including healthcare costs, lost productivity, and reduced quality of life for both patients and their caregivers.
Varied Presentation and Challenges
Autoimmune diseases manifest in a multitude of ways, presenting with diverse symptoms and affecting different organ systems. This heterogeneity poses challenges in accurately identifying and diagnosing these conditions. Additionally, the overlap of symptoms with other diseases and the lack of specific biomarkers further complicate timely recognition and treatment initiation. Overcoming these challenges requires increased awareness, improved diagnostic tools, and interdisciplinary collaboration among healthcare professionals.
Recognizing the prevalence of autoimmune diseases and the difficulties associated with their diagnosis and management is crucial in providing early intervention and support for those suffering from these often invisible illnesses. By addressing the unique concerns and needs of individuals with autoimmune diseases, we can improve their overall well-being and alleviate the burden imposed by these complex conditions.
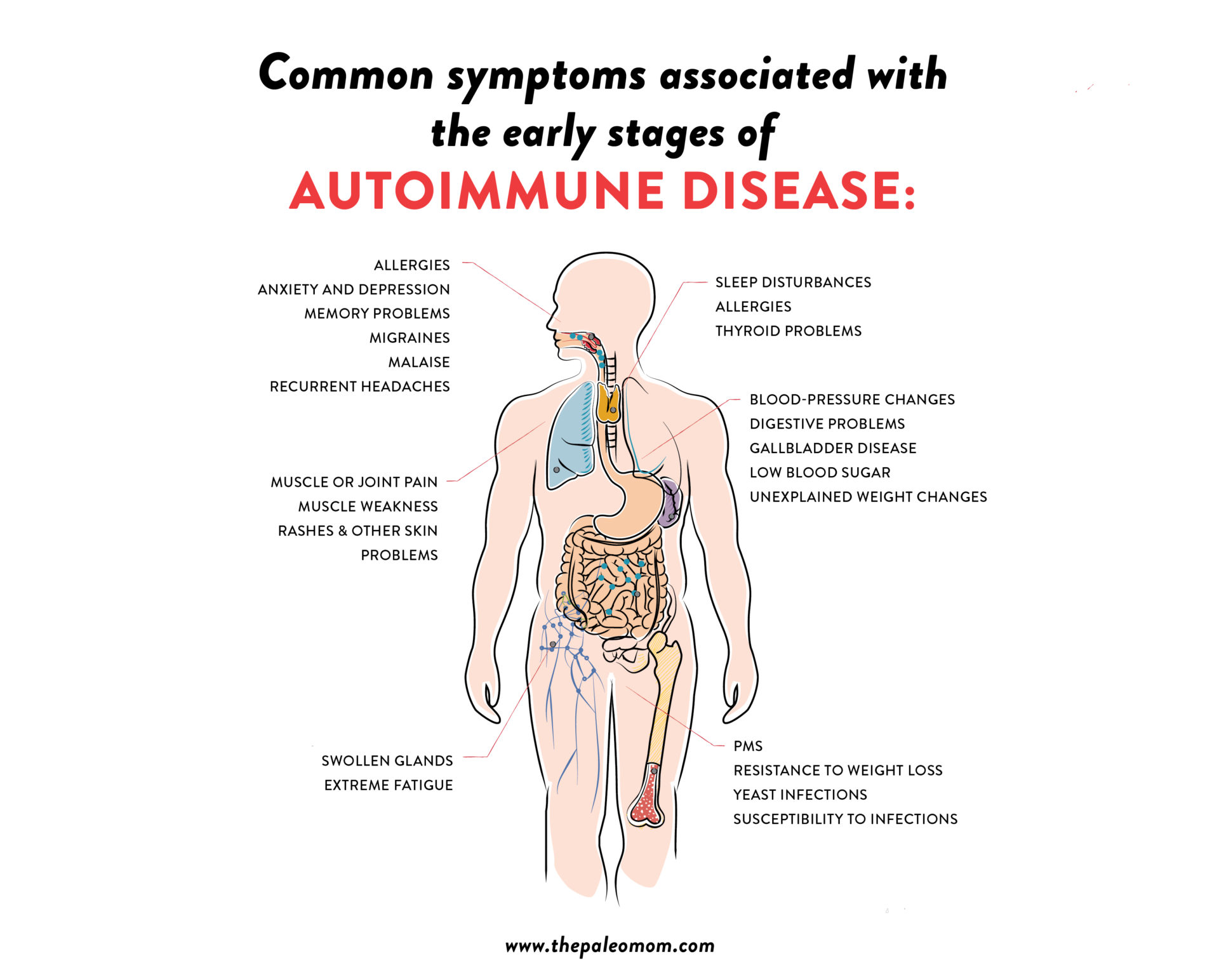
Identifying Common Symptoms
The ability to identify and understand the common symptoms associated with autoimmune diseases is crucial in early detection and proper management. Recognizing these telltale signs allows individuals to seek medical attention promptly and receive the necessary treatment. By being aware of the silent indicators that could be indicative of an autoimmune disease, individuals can take control of their health and well-being.
1. Fatigue: One of the most prevalent symptoms experienced by individuals with autoimmune diseases is persistent fatigue. This overwhelming sense of tiredness can significantly impact daily activities and productivity levels. It is important to pay attention to chronic fatigue that is not relieved by rest or sleep, as it could be a potential warning sign of an underlying autoimmune condition.
2. Joint Pain and Swelling: Inflammation of the joints is a common symptom shared by many autoimmune diseases. Persistent joint pain and swelling, especially in the hands, wrists, knees, and ankles, should not be ignored. The presence of these symptoms may indicate an inflammatory autoimmune condition, such as rheumatoid arthritis or lupus.
3. Skin Issues: Various autoimmune diseases can affect the skin, causing a range of symptoms such as rashes, hives, and redness. These skin manifestations can be a clear indication of an underlying autoimmune condition. Paying attention to any unexplained changes in the skin’s appearance or texture can aid in the early identification of autoimmune diseases.
4. Digestive Problems: Autoimmune diseases often affect the digestive system, leading to symptoms such as abdominal pain, bloating, diarrhea, and constipation. These gastrointestinal issues, especially when persistent or recurring, may be signs of conditions like Crohn’s disease, ulcerative colitis, or celiac disease. Seeking medical advice for proper diagnosis and management is essential in these cases.
5. Hair Loss: Experiencing excessive hair loss or thinning can be a distressing symptom associated with autoimmune diseases such as alopecia areata or Hashimoto’s thyroiditis. Paying attention to changes in hair texture and volume is important to identify any underlying autoimmune condition that may be causing the hair problems.
While these symptoms can be indicative of autoimmune diseases, it is important to note that the presence of one or a combination of these symptoms does not necessarily mean an individual has an autoimmune condition. Consulting with a healthcare professional is essential for proper diagnosis and treatment. Early detection and intervention can significantly improve the quality of life for individuals living with autoimmune diseases.
Unexplained Fatigue: A Subtle Warning Sign
Experiencing constant weariness without an apparent cause can serve as an important indicator of an underlying health issue. Fatigue that persists despite ample rest and lack of physical or mental exertion may be a subtle warning sign of an autoimmune disease, signaling the potential presence of an undiagnosed condition.
Unexplained fatigue refers to a state of persistent tiredness that cannot be attributed to everyday factors such as inadequate sleep, excessive physical activity, or emotional stress. It is a weariness that lingers and fails to dissipate even with proper rest and relaxation. The key characteristic of this fatigue is its unpredictability and prolonged nature, oftentimes accompanied by other non-specific symptoms that lead to a sense of physical and mental sluggishness.
While it is important to note that fatigue can be a symptom of various medical conditions, it is particularly significant in the context of autoimmune diseases. These conditions, characterized by an abnormal immune response targeting healthy cells and tissues, can cause the immune system to become overactive and dysfunctional. This immune dysregulation can result in systemic inflammation, leading to a range of symptoms, including unexplained fatigue.
Recognizing fatigue as a potential warning sign of an underlying autoimmune disease is crucial, as early detection and intervention can greatly improve the patient’s quality of life. Seeking medical attention and undergoing comprehensive evaluations can help identify the specific autoimmune condition causing the fatigue and initiate appropriate treatment strategies. As fatigue can manifest differently among individuals, it is important to communicate any unexplained weariness to healthcare professionals, enabling them to conduct a thorough assessment and provide tailored care.
In conclusion, unexplained fatigue should not be dismissed as mere tiredness. It can serve as a subtle warning sign of an autoimmune disease, beckoning individuals to pay attention to their overall health. By recognizing and addressing this symptom promptly, individuals can take steps towards a timely diagnosis and management of their conditions, ultimately leading to improved well-being and quality of life.
Persistent Joint Pain: Uncovering the Root Cause
Exploring the underlying factors contributing to ongoing joint discomfort.
- Understanding the possible origins of lingering joint pain.
- Identifying the hidden triggers that may be responsible for persistent discomfort.
- Investigating the potential connection between lifestyle choices and chronic joint pain.
- Examining the impact of inflammation on joint health and mobility.
- Exploring the role of genetics in the development of ongoing joint pain.
Uncovering the root cause of persistent joint pain is essential in order to effectively address and manage this debilitating condition. By gaining a comprehensive understanding of the various factors that may contribute to ongoing discomfort, individuals can take proactive steps towards finding relief and improving their quality of life.
Skin Problems: When Autoimmunity Takes Its Toll
Experiencing various skin problems can be a telltale sign of the impact autoimmunity can have on the body. When the immune system mistakenly attacks healthy cells and tissues, it can result in a range of skin issues that bring discomfort and affect daily life. In this section, we will explore the connection between autoimmune diseases and skin problems, highlighting the importance of recognizing these symptoms and seeking proper medical attention.
Autoimmune-related skin problems encompass a diverse range of conditions, each with its own unique characteristics and manifestations. These skin issues can manifest as rashes, hives, itching, redness, flaking, or blistering, among others. While the specific symptoms may vary depending on the underlying autoimmune disease, they often share commonalities in terms of their impact on the skin’s appearance and overall health.
One prevalent autoimmune-driven skin condition is psoriasis, which causes rapid skin cell growth, leading to the formation of red, scaly patches. Another common skin problem associated with autoimmunity is dermatomyositis, characterized by a distinctive rash and muscle weakness. Additionally, lupus, an autoimmune disease, can result in a butterfly-shaped rash on the face and skin sensitivity to sunlight.
| Common Autoimmune Skin Problems |
|---|
| Psoriasis |
| Dermatomyositis |
| Lupus |
Understanding these skin problems and their potential connection to autoimmune diseases is vital for prompt diagnosis and proper management. By recognizing the early signs and symptoms, individuals can seek timely medical intervention and receive appropriate treatment to alleviate discomfort and prevent further complications. Consulting with healthcare professionals who specialize in autoimmune diseases and dermatology can play a crucial role in accurately identifying and addressing these skin issues.
Moreover, raising awareness about the impact of autoimmunity on the skin is essential for destigmatizing these conditions and promoting empathy and support within communities. Individuals affected by autoimmune-related skin problems should feel empowered to discuss their experiences openly, seek the necessary medical assistance, and connect with support networks that can provide guidance and understanding.
In conclusion, skin problems serve as visible indicators of the toll autoimmunity takes on the body. Acknowledging and recognizing these symptoms allows for early intervention, appropriate treatment, and improved quality of life for individuals affected by autoimmune diseases. By shedding light on this aspect of autoimmunity, we can foster greater understanding and support within society, ultimately paving the way for enhanced care and breakthroughs in research.
Diagnosing Autoimmune Diseases
The process of identifying and diagnosing autoimmune diseases involves a careful evaluation of various factors that can indicate the presence of these conditions. It requires a comprehensive examination of symptoms, medical history, and laboratory tests to establish a proper diagnosis.
When it comes to recognizing potential autoimmune diseases, medical professionals rely on a combination of subjective and objective indications. Patients may experience a wide range of symptoms, such as fatigue, joint pain, skin problems, and digestive issues. These signs, although non-specific, can serve as early warning signals of an underlying autoimmune condition.
An accurate diagnosis typically involves a thorough examination of a patient’s medical history. This helps in identifying any genetic predispositions or previous illnesses that may contribute to the development of autoimmune diseases. Additionally, assessing the duration, frequency, and severity of symptoms can provide important insights into the possible presence of an autoimmune disorder.
While symptoms and medical history pave the way for suspicion, laboratory tests play a crucial role in confirming or ruling out autoimmune diseases. Blood tests, for instance, can measure the levels of certain antibodies associated with specific autoimmune conditions. These tests can provide objective evidence to support a diagnosis and guide further treatment options.
In some cases, additional diagnostic tools may be necessary. Imaging techniques, such as X-rays or MRI scans, can help visualize any potential damage caused by autoimmune diseases to organs or tissues. Biopsies, on the other hand, involve taking a small sample of affected tissue for further analysis under a microscope, aiding in the identification of specific autoimmune disorders.
Ultimately, the accurate and timely diagnosis of autoimmune diseases is crucial in order to provide patients with appropriate medical interventions and improve their quality of life. The combined evaluation of symptoms, medical history, and laboratory tests allows healthcare professionals to recognize the telltale signs of autoimmune diseases and offer tailored treatment plans for affected individuals.
Questions and answers
What are some common signs and symptoms of autoimmune disease?
Some common signs and symptoms of autoimmune disease include fatigue, joint pain and stiffness, muscle weakness, skin rashes, unexplained weight loss, fever, and trouble concentrating.
How are autoimmune diseases diagnosed?
Diagnosis of autoimmune diseases often involves a combination of medical history, physical examination, and specific blood tests to check for the presence of certain antibodies or markers associated with autoimmune conditions. In some cases, additional tests such as imaging or biopsy may be necessary.
Can stress worsen symptoms of autoimmune disease?
Yes, stress can worsen symptoms of autoimmune disease. Chronic stress may negatively affect the immune system, leading to increased inflammation and exacerbation of symptoms. It is important for individuals with autoimmune conditions to manage their stress levels effectively to minimize symptom flare-ups.
Are autoimmune diseases hereditary?
There is a genetic predisposition for developing autoimmune diseases, meaning that having a family history of autoimmune conditions increases the risk. However, it is not solely based on genetics, as environmental factors and lifestyle choices also play a role in the development of autoimmune diseases.
Can autoimmune diseases be cured?
Currently, there is no cure for autoimmune diseases. Treatment aims to manage symptoms, reduce inflammation, and prevent further damage to affected organs or tissues. This usually involves a combination of medication, lifestyle modifications, and sometimes therapy or counseling to help individuals cope with the challenges of living with a chronic condition.
What are the symptoms of autoimmune diseases?
The symptoms of autoimmune diseases vary depending on the specific condition, but some common symptoms include fatigue, joint pain, muscle aches, unexplained weight loss or gain, skin rashes, hair loss, and digestive issues.
How are autoimmune diseases diagnosed?
Autoimmune diseases can be challenging to diagnose as they share symptoms with other conditions. Doctors typically begin with a comprehensive medical history review and physical examination. They may also order blood tests to check for specific antibodies and inflammatory markers. In some cases, further tests such as imaging or biopsies may be required to confirm a diagnosis.
Are autoimmune diseases hereditary?
There is evidence of a genetic predisposition to certain autoimmune diseases. Having a family member with an autoimmune condition may increase the likelihood of developing one. However, genetics alone do not determine the development of an autoimmune disease, as environmental factors also play a significant role.
Can stress trigger autoimmune diseases?
While there is no definitive proof that stress directly causes autoimmune diseases, it is believed to be a contributing factor. Chronic stress can weaken the immune system and disrupt the body’s natural balance, potentially increasing the risk of developing an autoimmune condition or worsening existing symptoms.
What are the available treatments for autoimmune diseases?
Treatment for autoimmune diseases aims to manage symptoms, reduce inflammation, and suppress the immune system. Treatment options may include medication, lifestyle modifications, physical therapy, and alternative therapies such as acupuncture or herbal remedies. The specific treatment plan will depend on the type and severity of the autoimmune disease.